Physiotherapy assessment and treatment is often associate with sports injuries, surgeries and car accidents. While all these things are true, physiotherapists also treat more than this.
Physiotherapists treat aches and pains associated with occupations. Many of these involve repetitive movements and falls.
Our North Oakville Physiotherapists also treat repetitive strain types of pains associated with playing musical instruments. Injuries or pains can happen when weeks of rest have been taken and then practice, playing, and performing has increased. Changes to the instrument played, when practice and playing time is significant can also make a difference in how the body responds. This may be a new guitar with fret differences or having a new setup for your drums.
Maintaining your body for your music is helpful whether you play for fun or a profession.
Singing
Breathing is an important aspect of singing as well as wind instruments. Being able to fulling inhale and expand your ribcage and real your abdomen allows for full lung expansion and recoil for sound. Pain, stiffness, or dysfunction along this pathway can impact your singing.
Accessory muscles to breathing include some of our neck muscles. These muscles can help move our upper ribs. Some of our neck muscles also help with opening the mouth and supporting the vocal cords. Having strength, endurance and mobility in the area is important for singing.
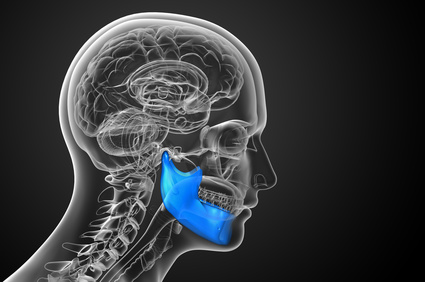
TMJ. The tempero-mandibular joint allows us to open wide to produce sound. The surrounding facial muscles help us modify our mouth shape for different vocalizations. Having this joint move well and the muscles have strength but limited tension allows for our best singing sounds. Think of the warmup exercises to “loosen the face”.
Physiotherapists can assess for range of motion and function of these areas. We can review proper breathing techniques, help loosen joints and muscles. Physiotherapists can also help with a home program of self care to maintain function allowing you to avoid musical related injuries and even assist with the craft.
Drums
Playing the drums is very physical. Having strong core and shoulder girdle muscles is helpful when playing for long periods of time. The low back wrists, hands and elbows are also areas that can be affected from drumming.
Strength – Having core strength and endurance allows for the low back to be more protected when sitting for log periods playing the drums. When muscles are strong further up the chain in the chest and shoulders, it supports the muscles and joints further down the chain.
Mobility – playing in a way that is strong but loose / mobile is a way to be more efficient with for and effort. Taking time for drills and learning helps with this.
Set-up – having and video of your drum setup or pictures where you look at your playing critical may help with strategies for ergonomic setup. Having lessons where your positioning and technique is looked at is also helpful.
Guitar
There are many factors in injuries and aches and pains associated with guitar playing. The weight of the guitar or bass, the strings, the frets, having a strap etc.
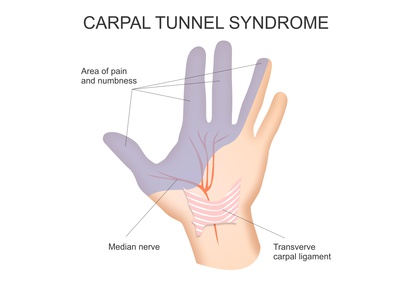
Hand, wrist, and elbow injuries can be common with guitar playing. Changes in the guitar or changes in the amount of time spent playing, or a combination of the two can impact injuries.
Physiotherapists may give mobility exercises for hand and wrist tendons as well as self care for the areas. Strengthening the small muscles of the hands and adding a stretching routine may be helpful as well.
It is always best to be assessed to ensure a physio treatment plan is designed just for you.
Why Physio?
Physiotherapists can assess for range of motion and function of these areas. We can review proper breathing techniques, help loosen joints and muscles. Physiotherapists can also help with a home program of self care to maintain function allowing you to avoid musical related injuries and even assist with the craft.
Contact us to book an appointment for Physiotherapy to address your musical related aches and pain.