Not all back pain is the same, so why would you follow generic exercises online?
Having a personalized Physiotherapy assessment allows your Physiotherapist to provide you with specific advise and specific exercises tailored for you and your issues. Whether it’s pain, stiffness, weakness, we are here for you.
A physiotherapist will often work in collaboration with a Registered massage therapist or acupuncturist to help you optimize your recovery or management.
There are many structures in your back that can lead to your pain or discomfort.
Muscles- skeletal muscle help with movement. They can also help with stiffness (think someone trying to push you over). There are muscles that help with both. The muscles can be injured through getting pulled or a strain. It maybe from asking them to produce more force then they are able to all at one time (like lifting a car tire) or from repeated smaller lifts that make the muscles tired and can injure them at lower levels (shovelling dirt in the garden). The low back muscles can spasm or tighten aggressively to protect themselves or the other structures around them.
Joints – our spine is made of multiple joints. They slide over one another to provide movement when the muscles pull on the bones they are attached to. They help absorb force as well. In the low back the joints help with more flexion and extension (forward and backward bending), in the upper back the joints allow more rotational movements. The joints of the spine are largest in the low back around the pelvis because they are responsible for carrying more weight. They are smallest in the neck or cervical spine. When a person does head stands they are putting more force on these joints that was intended by our evolutionary development. Joints may, but not necessarily cause us pain when they have arthritis, they can also become acutely sore with a sudden injury like a car accident.
Discs- the discs are between the bodies of the vertebrae. They help absorb force and keep the joints nicely spaced apart. They give nutrition to the vertebral bodies above and below them. The outside of the disc is called the annulus it is very strong. Discs in the low back tend to be injured with heavy lifting type injuries that our bodies are not prepared for or when fatigued.
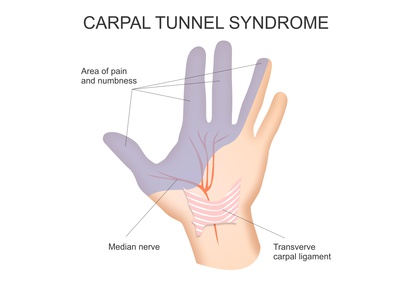
Nerves – nerves send messages to and from the spinal cord and brain. They are generally irritated or injured with compression force, stretch (burner or stinger), or chemical irritation (inflammation). They are involved in sending pain messages. If the spinal nerve roots have one of the above issues, we can have motor (muscle strength /control) problems and /or pain /numbness in the area that those nerves supply.
Brain-your brain is the keeper and senser or information. It is closely involved in how we experience pain. 2 people can have the same issue and have a very different pain experience. It’s important to address our thoughts and feelings about our pain and injury and how it affects our life. Previous life experience can also drive pain.
Organs – our organs actually have little local sensation and rather send messages further away. This is called visceral pain. Then most well known is probably the experience of a heart attack. It can be felt in the mid back, jaw, left shoulder and arm etc. When pain doesn’t make sense with a Physiotherapists assessment they will with your permission send information back to your primary health practitioner for potentially a closer look by them.
These sources of pain do not happen in a vacuum. Often there are a variety of sources of discomfort and one main driver.
Your physio helps distinguish which is the driver of your issue and provides a treatment plan. Their role is to help in the acute (fresh /new) stage and help with function and management beyond that.
Once you have had an injury or issue it is often true that it is more likely to happen again. This does not mean that you are damaged forever, or that you have a “bad back”.
This may be because a person doesn’t optimize recovery and maintenance. Physiotherapists and massage therapists can help you with this.
Read our next blog post for tips on optimization.
Remember, not everyone is the same what works for you may not be of benefit to the next person. This is why an individualized assessment and treatment plan is important.
Contact us to get started with one of our North Oakville Physiotherapist’s, Acupuncturist and Registered Massage Therapists (RMT) (905) 582-9700