If you are human, you likely have at one point or another experienced physical pain! Often, with some rest and time to heal, the pain goes away.
Sometimes it takes longer and you may need medication, or help from a health care practitioner (e.g. physiotherapist, chiropractor, massage therapist, etc.). One of the main drivers that brings people to us as Physiotherapists and Massage Therapists, is pain. People often seek the help from Physiotherapists when pain is inhibiting them from doing activities they enjoy or need to do.
Sometimes, that pain lasts much longer than the regular timeframe for tissue healing, and the different therapies you’ve tried did not successfully resolve your pain…
What does that mean?
Today, we will break down some basics of Pain to hopefully get a clearer grasp on what it is and where it’s coming from! (Then, in Part 2, we will discuss how all of this relates to Chronic Pain!)
Pain Defined
First, let’s start with the definition of pain… The most widely recognized definition is by the International Association for the Study of Pain (IASP):
“Pain is unpleasant sensory or emotional experience associated with actual or potential tissue damage, or described in terms of such damage.”
Let’s delve into that definition a bit more…
When understanding what pain is, it’s important to understand the difference between Input and Output to and from the brain:
- Input – sensory nerves send information to the brain regarding touch, sight, hearing, taste, and smell. The brain receives this information, interprets it, sorts and prioritizes it, then responds to it.
- Output – the brain responds to the input information with sensory experience (e.g. gentle touch, pain, heat, cold, etc.). That is to say, it decides based on the input information what that sensory experience feels like! It also responds with decision-making, problem-solving, emotions, blood pressure, and social behaviour. Some of these are conscious actions but some are unconscious.
In other words, your brain decides if something is painful or not. It controls the level of pain you experience and attaches an emotional response to it. Sometimes pain is meant to be protective to “potential tissue damage” as described in the above definition, because your brain has decided that certain movements or activities are risky.
In other words, you don’t need tissue damage to have pain!
And vice versa… sometimes you have can have tissue damage and no pain. For example, when you cut yourself, though it may hurt quite a lot initially, after you’ve bandaged it you likely forgot about it very quickly. The tissue is still damaged and healing, but your brain no longer sees the need to prioritize that information or continue letting you know about it. So, you no longer feel the pain!
Soul Surfer Bethany Hamilton speaks of losing an arm in a shark attack and not experiencing pain. How does this happen? Why do some people who lose limbs have phantom pain in the limb that is gone, and why do some not have this same experience?

Types of Pain
As Physiotherapists we often will ask our patients more questions about their pain. When did your pain start? What does it feel like? Where is it located? How much pain? What makes the pain better? What makes the pain worse?
- Nociceptive Pain:
- most common type of pain, often described as: sharp and intense, and later on more achy, dull, or throbbing
- comes from specific tissue injury, or the potential for such injury (e.g. hand on hot stove: you get the warning pain to move your hand away before actual tissue damage occurs)
- usually goes away once the injury has healed
- can be due to the inflammatory process (responds well to anti-inflammatories)
- can be due to mechanical factors (specific movements make it worse while others make it better)
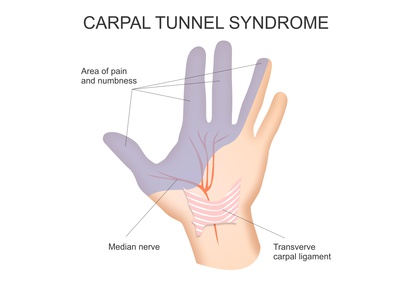
- Peripheral Neurogenic / Neuropathic Pain:
- Nerve pain, often described as: burning, shooting, electrical jolts, aching, nagging, throbbing, or piercing / sharp. Can also have associated numbness or tingling / crawling sensations.
- Pain often radiates away from the site of injury, usually into the limbs. Therefore, where the pain is felt is not always where the cause is!
- Can be due to the altered mechanics of the peripheral nervous system, including a pinched nerve
- Can also have inflammatory and mechanical components, like nociceptive pain
- Visceral Pain
- Experiencing pain from our organs in different areas of the body.
- Heat attacks or angina is often felt in the left jaw, the left mid back, left arm
- Central Nervous System (CNS) Sensitization Pain
- This type of pain tends to be more chronic (but not always), often described as burning, stabbing, shooting, nagging.
- Pain location is more dispersed and not as localized
- Pain intensity does not usually match the activity or triggering factor (i.e. it’s more sensitive than would be reasonably expected)
- Symptoms do not always respond well to medication
- Symptoms do not have clear inflammatory or mechanical components (i.e. the pain is not always related to activity, position or posture)
- More likely to be affected by anxiety, stress, and/or emotional state (these affect all the types of pain, but tend to be more predictive CNS pain)
- More likely to affect sleep quality (although, sleep quality can be affected by all the types of pain)
It is important to keep in mind that pain is multi-faceted and complex.
It is possible to have two or all of the types of pain going on at the same time.
If dealing with both nociceptive and neurogenic, the neurogenic pain will be more predominant. If dealing with both neurogenic and CNS sensitization pain, the sensitization will be more predominant.
Based on the above definitions, can you identify what kind(s) of pain you are experiencing or have experienced?
What does it all matter anyway?
The type(s) of pain you are experiencing, along with how it all started, how it’s affecting you currently (both physically and emotionally), and what your goals and hopes for Physiotherapy are, all play a role in determining your treatment plan!
For one, treating the cause is important and the type of pain can help us identify what that is.
Secondly, treatment is not one-size-fits-all. What works for one person may not work for another.
Lastly, each of us is a whole human being, not just a collection of parts. Therefore, for the most effective results it is important to treat the whole person rather than just where the pain is felt. That includes overall quality of life, any and all contributing factors that may be driving the issue, and ultimately, what it is you want to get out of treatment.
We can help so many people who are experiencing pain. Physiotherapists understand your activities, your injuries and your goals. As Physio’s we work with you to reach your goals whether that is decreased pain, increased function, getting back to activities of enjoyment, and being empowered with your actions and choices. At Palermo Physio and Wellness in Oakville Ontario we want to work with you and support you. While much of what we do during a “hands-on” session is helpful, the real magic happens with what education we give you and your home program!
If you see a practitioner and they haven’t gotten you started with some form of movement, breathing, exercises, this is a problem.
Our Oakville Ontario Physiotherapists have been able to extend our reach as we have transitioned to virtual or video Physiotherapy sessions. It is super easy and user friendly, just like a “FaceTime” or video conference chat. We are able to treat you anywhere in Ontario. Most insurance companies cover these types of Physio sessions.

If you are interested in a FREE 10 minute consult to see how we can help you reach your goals please contact us info@palermophysio.ca
Stay tuned for part 2!

