School has officially begun for the year and with that comes an increase in activity levels for many children. As the fall and winter season approaches, many kids will participate in school sports as well as extra-curricular organized sports and activities. This ramp-up in exercise levels can sometimes lead to aches and pains, particularly in young children who are still growing at fast rates.
The term “growing pains” refers to this sort of injury. This pain is muscular in nature and occurs because bones are growing and changing at a faster rate than the muscles can keep up, which puts added stress and tension on the muscles. This can be more prevalent in children who participate in sports all year long, or children who play multiple sports at the same time.
Common Growing Pains
- Sever’s Disease: pain in the back of the heel where the Achilles tendon attaches.
- Shin Splints: pain in and around the shins.
- Osgood Schlatter’s Disease: pain below the knee from the quadriceps muscle pulling on the shin bone.
Symptoms of Growing Pains
- Pain in the thighs, knees, shins, or ankles.
- Pain after playing sports or engaging in activity.
- Pain at night when sleeping.
- Pain is described as an “ache” or “burning.”
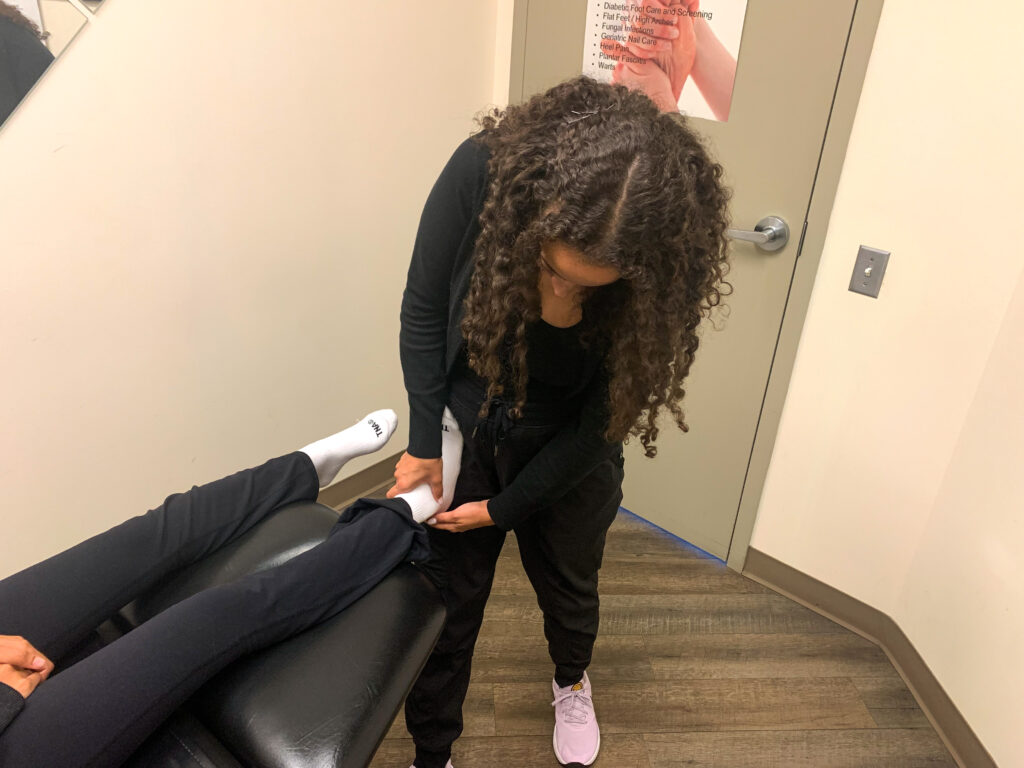
Physiotherapy and Growing Pains

Physiotherapy treatment is a very effective way to treat and manage activity-related pains in growing children. The aim is to reduce inflammation and improve muscle flexibility and strength. This includes techniques like mobilizations, manual stretching, and soft tissue work. The physiotherapist can also instruct you on how to manage your symptoms at home and what exercises to do to effectively target the area.


If your child is experiencing pain and discomfort with exercise, book an initial assessment here with one of our physiotherapists. They will design a treatment program individually tailored to your child’s needs, age, and activity level.